Addressing the Ohio Health Crisis – Our Response to the 2024 HPIO Dashboard
Table of Contents
Why are We Writing this Ohio Health Dashboard Breakdown & Response?
At the Institute of Family and Community Impact, we take action for community and family health. This includes advocating for policies that improve the overall health and well-being of everyone we serve. First, we must accessibly breakdown and disseminate information about our community health and well-being, to advocate for change.

To achieve our purpose at IFCI, we believe in the power of knowledge and awareness spread through continuous learning. By effectively breaking down complex information and making it accessible to all, we seek to empower individuals and communities to make informed decisions about what’s going on in our communities. The Health Policy Institute of Ohio’s (HPIO) biennial 28-page report presents everything you need to know about Ohio’s health value as of 2024, and it’s contents directly impact the work we do here at IFCI. So, what better way to inform the community than to respond to this report with what we learned, expand and breakdown some of the information they shared, possible solutions, and more!
We’ll continue collaborating locally and beyond with healthcare providers, community stakeholders, and policymakers on evidence-based solutions that address key behavioral health challenges like the ones we explore today. As an initiative of OhioGuidestone, one of the largest behavioral healthcare providers in the state, we’re in a unique position to address these challenges. We envision a healthier, informed and empowered community where everyone has the resources and support they need to thrive.
We apply HPIO’s 2024 Health Value Dashboard to the extensive research we have done on Ohio behavioral health needs throughout the years, and also apply it to the innovative work we do here at IFCI. Although we recognize the severity of the health disparities that exist, and the systemic and structural need for improvement in our health value, we also remain hopeful in a future where suffering in our communities lessens.
What We Know:
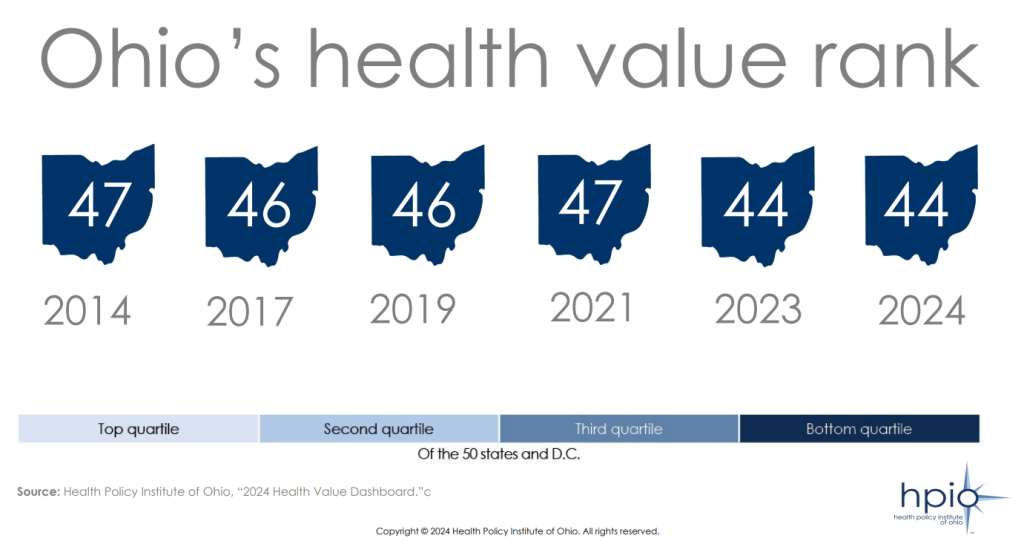
As of 2024, Ohio is positioned 44th out of 50 states (and D.C). in terms of our health value. But what exactly is health value? Health value is the combination of population health and what we spend on healthcare. This ranking indicates that Ohio residents live less healthy lives and spend more money on healthcare compared to individuals in the majority of other states.
Social Drivers & Ohio Health
Ohio ranks in the bottom quartile for health value. Various factors affect this ranking, with social drivers of health at the forefront of perpetuating health disparities. It is crucial to promptly address this issue by presenting evidence-based solutions, particularly focused on addressing social drivers. By focusing on these social drivers and implementing targeted interventions, we can begin to bridge the gap and improve our overall Ohio health value.
HPIO pinpointed the following modifiable factors contributing to Ohio’s health value score:
- Access to care
- Healthcare system
- Public health and prevention
- Social and economic environment
- Physical environment
Minoritized Populations are Being Disproportionately Impacted
Minoritized populations like Ohioans of color, Ohioans with low incomes, Ohioans with disabilities, Ohioans with less education, LGBTQ+ Ohioans, and those living in rural and Appalachian areas continue to face barriers to health where they live, work, and play.
These barriers can include limited access to healthcare services, higher rates of chronic health conditions, inadequate health education, stigma, and discrimination within the healthcare system.
Black Ohioans

Did you know racism is a primary social driver of poor health outcomes experienced by Black Ohioans? Racism is a system, built and held up by practices and policies that result in the unfair distribution of resources, power, and opportunity. It is due to this systematically engrained racism, that Black Ohioans often experience worse outcomes than white Ohioans across measures of health, healthcare access, and the social, economic and physical environment.
Examples of racist policies and systems that contribute to Ohio health gaps in outcomes:
- Discrimination and unfair treatment across systems (i.e., healthcare organizations, academic institutions, etc.)
- Divestment in public transportation and education
- Redlining and zoning policies
- Explore our Maternal Vitality innovation to learn more about how racism impacts maternal and infant mortality and morbidity rates.
When HPIO Explored the Difference in Ohio Health outcomes between Black and white Ohioans, what did the data show?
-Black Ohioans are 13.7 times more likely to be treated worse in healthcare due to race.
-Black Ohioans are 2.7 times more likely to experience infant mortality, and 1.6 times more likely to experience a premature death.
-Black Ohioans are 5.7 times more likely to experience incarceration than their white counterparts.
-Black children in Ohio are 9.4 times more likely to receive unfair treatment due to their race, and 3.5 times more likely to experience food insecurity in their childhood.
Data source: HPIO 2024 Ohio Health Value Dashboard
What would Black Ohioans Health Look Like if Disparities were Eliminated in Ohio?
-If racist healthcare disparities were eliminated, 189,344 fewer Black Ohioans would experience racism when seeking healthcare.
-If racist criminalization disparities were eliminated, 16,973 fewer Black Ohioans would be incarcerated.
-If racist healthcare policies and practices regarding infant mortality and morbidity were addressed, 60,004 fewer years of life would be lost by Black Ohioans.
Data source: HPIO 2024 Ohio Health Value Dashboard

Hispanic, Latino and Asian Ohioans
Racism is a primary driver of the adverse health effects faced by Hispanic, Latino, and Asian Ohioans. Hispanic/Latino individuals in Ohio experience worse outcomes in healthcare access and in their social, economic, and physical environments compared to white, non-Hispanic Ohioans. Similarly, Asian Ohioans also experience worse outcomes in healthcare and in their, physical and social environment compared to their white counterparts.
For Ohio health to improve, racism and it’s impact on the health of minoritized racial groups, must be addressed.
What were the Difference in Outcomes for Hispanic/Latino and Asian Ohioans when Compared to white Ohioans?
-Hispanic individuals are 4.6 times more likely to experience physical symptoms as a result of experiences of racism.
-Asian children are 9.4 times more likely to experience unfair treatment due to their race.
Data source: HPIO 2024 Ohio Health Value Dashboard
If Disparities were Eliminated what would Hispanic/Latino and Asian Ohioans Health Look like?
-If the racism causing physical symptoms in Hispanic Ohioans was eliminated, 19,486 fewer individuals would experience these physical symptoms.
-If racist unfair treatment of Asian American children in Ohio was eliminated, 6,051 fewer Asian children would experience this treatment.
Data source: HPIO 2024 Ohio Health Value Dashboard
Ohioans with Lower Incomes and/or Less Education
Ohio residents with lower educational levels and incomes tend to face worse outcomes across various health metrics, healthcare access, and the social, economic, and physical environment compared to those with higher education and income levels. The unequal distribution of resources limits opportunities and access for individuals in Ohio with lower incomes.
Ohio children living in families with lower incomes experience food insecurity 91.1 % times higher than Ohioans with higher incomes.
HPIO 2024 Ohio Health Value Dashboard
Food is a basic necessity, and the alarming reality of Ohio’s children going without an essential element of survival (food), is heartbreaking. It’s crucial for us to address food insecurity among Ohio’s children. No one, especially children should go without access to nutritious meals, ever. To increase food access for Ohioans experiencing food insecurity, or minoritized groups identified as being “at-risk” for lack of food access, we should implement various initiatives such as: the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) and Senior Farmers’ Market Nutrition Programs.
LGBTQ+ Ohioans
In society, minoritized groups and their well-being are oftentimes ignored or overlooked resulting in a lack of data or substantial gaps in data. As an example, there’s a lack of available public data on the LGBTQ+ population estimate in Ohio. However, worldwide research has indicated that homophobia and transphobia significantly contribute to poor health outcomes experienced by LGBTQ+ individuals.
In research, being intentional in sampling minoritized social groups is necessary to improve data quality and reporting. The quick statistic from HPIO’s Ohio Health Value Dashboard, is just one of the stark disparities that LGBTQ+ Ohioans experience as worse than their heterosexual and/or cisgender counterparts across measures of social environment and health.
LGBTQ+ youth in Ohio are 4.8 times more likely to consider suicide than their heterosexual or cisgender peers.
HPIO 2024 Ohio Health Value Dashboard

Ohioans Living in Rural or Appalachian Areas
As a minoritized group, Ohioans living in rural or Appalachian areas often receive the same lack of data representation that groups like LGBTQ+ Ohioans experience. However, as the gut-wrenching statistic on heart disease rates in rural Ohio counties shows, there is an imminent need to address the disparities faced by Ohioans in these geographical locations. Pushing rural and Appalachian Ohioans to the outskirts of our minds as a society, further pushes them away from the health resources they need to thrive.
Heart disease death rates among working-age Ohioans were highest in rural and Appalachian counties in 2021-2022. Mercer County had the highest rate of heart disease, at 272.5 per 100,000 population, which is 40% higher than the overall state rate of 194.8
HPIO 2024 Ohio Health Value Dashboard
The American Heart Association (AHA), explored health disparities of people in rural America as being another one of the unique challenges this minoritized group faces in our society. Free data from the American Heart Association and American Stroke Association identified some key factors that are contributing to the negative health outcomes among people in rural areas, including:
- Physical access to healthcare
- Accessing various healthcare providers, such as clinical and mental health professionals is often extremely challenging in rural areas. This difficulty is exacerbated by geographical terrain and a shortage of local, convenient and accessible public transportation options.
- The opioid crisis
- Rural areas in the U.S. continue to experience more alarming rates of opioid drug use and overdose cases than their urban area counterparts.
- Social drivers of health
- As we have explored throughout this article, social drivers include: income, housing, food, transportation, and more. The lack of access to these needs in rural populations contributes to poor cardiovascular and other health outcomes.
Systemic Change is Necessary to Improve Ohio Health: Public Health Data & Minoritized Groups
As we explored the harsh realities that minoritized Ohioans face, we want to highlight the need for systemic level change to public health data. Without accurate statistics, it becomes difficult to implement targeted interventions and support systems for individuals who need them to improve Ohio health. It’s crucial to amplify the voices of minoritized groups. Their needs should not only recognized but also actively met to build a more equitable society. For minoritized social groups who get overlooked or ignored in data collection, there are many ways for us as a society to improve the quality and availability of publicly available data:
- Collecting consistent disaggregated data on:
- Race/ethnicity
- Age
- Income / education
- Geographical location
- Disability status
- Sexual orientation/gender identity
- Religion
- Other demographic categories.
- Oversampling groups with smaller population sizes to ensure that they are represented in the data:
- This also increases the ability to measure the experiences of Ohioans who are part of more than one systematically marginalized group.
- Providing local data at the county, zip code levels when this is possible, and also prioritizing training on how to collect demographic data to reduce missing data and potential non-response to collection.
- Historically, minoritized populations have been subject to violence in research, and data collection. Ensuring cultural responsiveness and competency of researchers who will be collecting, studying, and responding to this data is crucial to reduce further harming our communities.
Improving Ohio Health: Let’s Explore 2 of the Policy Priority Areas from HPIO:

We explore two of the four Policy Priorities presented by the Health Policy Institute of Ohio below in more-depth.
1. Mental Well-Being
Data representing Ohioans of all ages shows that mental health challenges are common. Even though the rate of adult depression has increased significantly in Ohio adults, one in every four Ohio Adults who needed mental health treatment did not receive it. Data from the CDC’s Youth Risk Behavior Surveillance System revealed that significant mental well-being disparities exist among Ohio teens, particularly for students assigned female at birth and students who are members of the LGBTQ+ community.
In 2021, 43% of overall Ohio high school students reported consistently feeling sad or hopeless. 76% of gay, lesbian or bisexual Ohio teen students reported consistently feeling sad or hopeless. Along with 56% of students assigned female at birth.
Youth Risk Behavior Surveillance System, Centers for Disease Control and Prevention (CDC)
Knowing the above disparities exist, HPIO explored the following solutions as possibilities for improving mental well-being among Ohioans. At IFCI, we thought it’d be important to expand on what these possible evidence-based solutions may look like in practice and how they may impact Ohio health.
- Improve access to telemental health services to positively influence Ohio health.
- Telemental health services improve access to care especially for individuals in areas with limited access to mental health care professionals such as those who live in rural communities like Appalachia.
- At IFCI, we do recognize more research is needed to confirm the effectiveness of telemental health services for those who experience minoritization and other barriers to accessing digital health interventions.
- Learn more about the importance of telehealth in behavioral healthcare by reading our telehealth-related Position Papers linked below.
- Fund programs with evidence of mental health benefits such as:
- Mental Health First Aid (MHFA)
- First, what is Mental Health First Aid? It is an evidence-based, early-intervention training course to help individuals with mental health or substance use disorders using MHFA’s five-step action plan. The curriculum has been adapted for diverse populations from youth to older adults to veterans. These 8-12 hour courses are filled with information for attendees, including how to recognize signs and symptoms related to mental health or substance use disorders and appropriate responses to situations that may come up. How could programs like this positively impact our Ohio health? Evidence-based curriculums like MHFA have the potential to increase common knowledge of mental health while reducing stigma.
- MHFA’s five-step action plan is:
- Assess risk of self-harm.
- Listen non-judgmentally.
- Reassure and share information.
- Encourage self-help.
- Encourage professional help.
- Mental Health First Aid (MHFA)
- Improve the behavioral health crisis system, including the 988 lifeline and mobile crisis response. This includes making sure that these services are funded and available across our state.
- By pouring into our Ohio behavioral health crisis system, (E.g., 988 lifeline and mobile crisis response), we commit to giving quick and vital support to individuals who need it, when they need it. We can also help to lower the stigma of getting help for mental health challenges and create a more compassionate, safe, and supportive community for all.
2. Creating Opportunities for Ohio Health to Thrive

Across some of our Ohio communities, there are a lack of resources, environments, and opportunities essential for communities to fully thrive. Stigma, discrimination, and poverty are examples of factors that create barriers like limited access to nutritious food, meaningful jobs, and secure housing. For example, Ohio’s ranking is 48 out of 51 for toxic pollutants, which accounts for factors such as the size of chemical releases, how chemicals move through the environment, and their toxicity.
Our Ohio health value is impacted by our environments, as can be shown in our bottom quartile outdoor air quality ranking. What does air quality have to do with our Ohio health? It starts with macro and micro power relations. Discriminatory policies and practices have shaped where Black and Brown Ohioans live and whether they even have access to safe neighborhoods free from harmful conditions, such as air pollution.
Historically, practices like redlining have resulted in disinvestment, concentrated poverty and depleted property value in neighborhoods where Ohioans of color live. Then, those areas were made vulnerable to industry and highway development, which continues to result in greater levels of air pollution even today.
Data showed Black, Asian or Pacific Islander, and Latino Ohioans were more likely to experience exposure to air pollutants than white Ohioans in 2020.
U.S. Environmental Protection Agency (EPA) data compiled by the National Equity Atlas
Knowing the impact of the above disparities on Ohio health, HPIO identified potential evidence-based solutions which we explore in more detail below.

- Increase the availability and accessibility of green spaces and parks that offer environmental and health advantages to our communities.
- Evidence supports the likelihood of achieving expected benefits/outcomes like: increased physical activity, improved mental health, and improved overall health outcomes with increased green spaces and parks in our communities.
- Oftentimes, minoritized social groups have less access to green spaces and parks. It is important to consider questions like this when we consider green space expansion to positively impact Ohio health:
- Which neighborhoods in our communities have numerous vacant lots, abandoned infrastructure, or underutilized recreation areas that have the potential to be converted into lively green spaces, trails, or parks?
- What partnerships could help developing and backing community-wide projects to enhance green spaces and tree coverage in neighborhoods impacted by redlining?
- What anti-displacement policies can we implement to safeguard our neighborhoods and communities from gentrification? How can unequal access to newly established green spaces and parks be prevented?
- What is the local policing and criminalization approach to our community public spaces, such as parks?
- How do these approaches harm minoritized individuals, families, and groups?

- Use Health Equity Impact Assessments (HEIA) to identify potential health impacts of proposed policies, services, and programs for systematically minoritized groups.
- The HEIA is a four-part health equity assessment that provides a more focused consideration of issues that affect health equity– social drivers of health and health disparities. What are the 4 features that an HEIA should include?
- Qualitative and quantitative methods and best available data sources.
- Input from stakeholders like healthcare organization leaders, community-based organizations, representatives of the community that may be impacted, and local government officials.
- Focus on the potential effects of a proposed policy, program, or project across other sectors of health.
- Recommendations to monitor and manage potential impacts.
- At IFCI, we believe HEIAs must be adopted by policy decision-makers to understand exactly how policies, projects, and programs affect our Ohio health and health equity. North Carolina, one of the states who has began utilizing HEIA’s has an HEIA implementation guide which could be helpful for Ohio health stakeholders to lean into when considering this potential evidence-based pathway to addressing the health disparities of minoritized groups.
- The HEIA is a four-part health equity assessment that provides a more focused consideration of issues that affect health equity– social drivers of health and health disparities. What are the 4 features that an HEIA should include?
Conclusion: Our Work at IFCI & Why We Care About Ohio Health
To address these disparities we have to offer robust and collaborative efforts toward quality healthcare, responsive health equity policies and procedures (that are reviewed and updated on an ongoing basis), cultural responsiveness in our providers, and empowering communities. Creating a more inclusive and equitable healthcare system that meets the diverse needs of all Ohioans will help us to build and support individuals, families, and communities to thrive.
Improving Ohio health across all domains should be our top priority as a state. Here at IFCI, it is. A lot of the work we do is already informed and will be further enhanced by the findings of the 2024 Ohio Health dashboard. What does the 2024 health dashboard have to do with who we are at IFCI? EVERYTHING!
As part of OhioGuidestone, we’ll continue to develop innovative, evidence-based solutions to reduce barriers to care, increase access to quality and responsive care, and improve outcomes for people with mental health and substance use disorders.
In our field of mental health, we need research to provide effective culturally responsive treatments, interventions, and practices for those with serious mental illnesses and needs. We also understand, that Ohio health is holistic, meaning the client in front of us is a whole-person with a wide range of complex needs. We’ve made it a priority to integrate research into our services via our Institute of Family and Community Impact. By utilizing evidence-based practices, backed by our own center of excellence, we make sure that our programs and interventions are grounded in the best available evidence in the field to inform our innovative expansion here.
We don’t just stop at developing innovative solutions. Through IFCI, we also continuously evaluate the effectiveness of our programs to identify potential areas where we need to improve to better serve people just like you! This is key to achieving better Ohio health outcomes for our clients and our communities.
By staying up to date on the latest research and continually seeking new, innovative and creative solutions, we are better equipped to address the complex challenges that arise in our communities; and by addressing these challenges we slowly work toward empowering our clients to improve their individual and family vitality.
We know that diverse collaboration in and beyond our Ohio borders is essential in creating sustainable solutions to address our Ohio health value and existing and evolving health disparities. It’s by working together to advocate for change that we will create a healthier and more equitable future for all Ohioans. Learn more about how our innovations are already working toward improving our Ohio health value and stay tuned in the future for more from us at IFCI.
Ohio Health Research Citation List
988 Suicide and crisis lifeline in Ohio. (n.d.). https://mha.ohio.gov/get-help/crisis-systems/988-suicide-and-crisis-lifeline-in-ohio/welcome
2021 YRBSS Data release available now. (n.d.). https://www.cdc.gov/healthyyouth/data/yrbs/index.htm
Green space & parks. (2023, May 5). County Health Rankings & Roadmaps. https://www.countyhealthrankings.org/strategies-and-solutions/what-works-for-health/strategies/green-space-parks
Harrington, R. A., Califf, R. M., Balamurugan, A., Brown, N., Benjamin, R. M., Braund, W. E., Hipp, J., Konig, M., Sanchez, E., & Maddox, K. E. J. (2020). Call to action: Rural Health: a presidential advisory from the American Heart Association and American Stroke Association. Circulation, 141(10). https://doi.org/10.1161/cir.0000000000000753
Health disparities among the many unique challenges for people in rural America. (n.d.). American Heart Association. https://newsroom.heart.org/news/health-disparities-among-the-many-unique-challenges-for-people-in-rural-america#:~:text=According%20to%20data%20reported%20in,who%20live%20in%20urban%20areas.
Health Policy Institute of Ohio. (2024, April). 2024 Health Value Dashboard. https://www.healthpolicyohio.org/our-work/facts-figures/2024-health-value-dashboard#:~:text=Ohio%20ranks%2044%20on%20health,and%2034%20on%20healthcare%20spending.
HEIA Implementation Guide | NCDHHS. (2024, January 25). https://www.ncdhhs.gov/heia-implementation-guide
Mental health first aid. (2019, January 25). County Health Rankings & Roadmaps. https://www.countyhealthrankings.org/strategies-and-solutions/what-works-for-health/strategies/mental-health-first-aid
Ohio 2019 BRFSS Annual Report. (n.d.). https://odh.ohio.gov/know-our-programs/chronic-disease/data-publications/ohio-2019-brfss-annual-report
Telemental health services. (2024, April 25). County Health Rankings & Roadmaps. https://www.countyhealthrankings.org/strategies-and-solutions/what-works-for-health/strategies/telemental-health-services
Trauma-informed schools. (2018, May 17). County Health Rankings & Roadmaps. https://www.countyhealthrankings.org/strategies-and-solutions/what-works-for-health/strategies/trauma-informed-schools
What is a Health Equity Impact Assessment (HEIA)? (2023, November 29). https://healthcare.rti.org/insights/health-equity-impact-assessment-on-programs-policy
WIC & Senior Farmers’ Market Nutrition programs. (2023, July 13). County Health Rankings & Roadmaps. https://www.countyhealthrankings.org/strategies-and-solutions/what-works-for-health/strategies/wic-senior-farmers-market-nutrition-programs

Payten Kleinhenz
Payten Kleinhenz B.S., CDCA is a Behavioral Health Specialist IV at OhioGuidestone. As a former Research Analyst at the Institute of Family and Community Impact, she helped lead applied clinical science & research communications. She authored department written content such as newsletters and reports, social media posts, and articles by prioritizing evidence-based, research-backed writing and reader accessibility. She also managed research data through data collection, entry and storage. Payten graduated with a B.S. in Sociology from Western Carolina University in May 2022. Her sociological background drives her passion for dismantling systemic and structural barriers. Payten’s primary research and professional areas of interests include substance use disorders, and family/social ties in the context of power relations and structures.